How do Mast Cells Impact Our Patients Health?
What are mast cells?
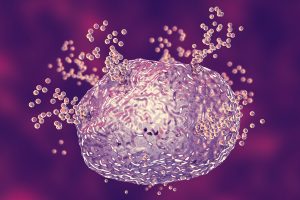
Mast cells are myeloid immune cells that are present throughout the body. They exist in areas that connect the external environment to the body, such as mucosal and epithelial surfaces. Connective tissue contains high amounts of mast cells. Inside mast cells are granules containing histamine, heparin, cytokines, chemokines, proteases, leukotrienes, and growth factors.1 Their primary mechanism of action is IgE-mediated allergic reactions through the FceRI receptor. When an antigen connects with a mast cell, it crosslinks two or more FceRI molecules, which activates the release of granules from the mast cell.2 Non-IgE mediated triggering of mast cells also results in the degranulation of mediators.
What role do mast cells play in the body?
Mast cells are an integral part of both the innate and the adaptive immune system, regulating other immune cells such as T cells, B cells, dendritic cells, macrophages, eosinophils, endothelial cells, and epithelial cells.1 Since they contain multiple different granules, they have many other physiological functions. Through the release of pro-angiogenic granules such as VEGF, mast cells are involved in increasing angiogenesis.3 Mast cells play a role in vasodilation, which is seen in different allergic reactions. They also play a role in vascular and bronchial homeostasis.
What is histamine intolerance?
Histamine intolerance is thought to be from a deficiency in the gastrointestinal diamine oxidase enzyme (DAO) that breaks down histamine.4 If the enzyme is decreased, then there are increased amounts of histamine in the GI tract that can cause nonspecific gastrointestinal and systemic symptoms. The DAO enzyme can be lower because of genetic causes and conditions that cause inflammation in the GI tract.5 Supplemental DAO enzymes can help increase the ability to break down histamine in the gastrointestinal tract but do not decrease the amount of histamine released from mast cells. DAO enzymes are localized in the digestive tract, as they are not systemic (meaning they do not impact mast cells throughout the body).
How do you naturally support healthy mast function?
One way to support healthy mast cell function is by supporting a healthy release of histamine from the mast cells. Flavonoids are a type of polyphenol compound that is found in many fruits and vegetables and are known to be anti-oxidants.8 Quercetin is one of the best-known flavonoids shown to support a healthy release of histamine from mast cells. Fisetin, perilla, and luteolin are also flavonoids that have been shown to support healthy levels of IgE-mediated release of histamine from mast cells.10,11,12
Another way to support healthy mast cell function is by supporting a healthy amount of histamine uptake. If histamine cannot reach its receptor, it cannot start the cascade of events leading to classic allergy symptoms. Pharmaceutical anti-histamines for nasal allergies and skin issues are medicine such as Benadryl® (diphenhydramine), which blocks the H1 receptor from histamine. However, natural histamine blockers can be used to support healthy uptake as well. Stinging nettle (Urtica dioica) has been shown to support healthy H1 receptors.14 Nigella sativa, commonly known as black cumin, has gastro-supportive effects, including decreasing stomach acid.15
Summary
Mast cells are very complex cells with both immunological and physiologic functions. The most well-known mediator is histamine which causes classic allergy symptoms. Fortunately, there are natural options to support healthy mast cell function systemically in the body.
References
- Krystel-Whittemore M. et al. Mast Cell: A Multi-Functional Master Cell. Frontiers in Immunology. Vol 6. 620.
- Sibilano R, Frossi B, Pucillo CE. Mast cell activation: a complex interplay of positive and negative signaling pathways. Eur J Immunol(2014) 44(9):2558–66.
- Norrby K. Mast cells and angiogenesis. APMIS(2002) 110(5):355–71.
- Schnedl WJ, Enko D. Histamine Intolerance Originates in the Gut. Nutrients. 2021;13(4):1262.
- Comas-Basté O, Sánchez-Pérez S, Veciana-Nogués MT, Latorre-Moratalla M, Vidal-Carou MDC. Histamine Intolerance: The Current State of the Art. Biomolecules. 2020;10(8):1181.
- Frieri M. Mast Cell Activation Syndrome. Clin Rev Allergy Immunol. 2018 Jun;54(3):353-365.
- Seneviratne SL, Maitland A, Afrin L. Mast cell disorders in Ehlers-Danlos syndrome. Am J Med Genet C Semin Med Genet. 2017 Mar;175(1):226-236.
- Shaik Y, Caraffa A, Ronconi G, Lessiani G, Conti P. Impact of polyphenols on mast cells with special emphasis on the effect of quercetin and luteolin. Cent Eur J Immunol. 2018;43(4):476-481.
- Weng Z, Zhang B, Asadi S, et al. Quercetin is more effective than cromolyn in blocking human mast cell cytokine release and inhibits contact dermatitis and photosensitivity in humans. PLoS One. 2012;7(3):e33805.
- Theoharides TC. Et al. Mast Cells and Inflammation. Biochimica et Biophysica Acta. 2012. 1822:21-33.
- Kazimerova l. et al. The effect of short -term and long-term application of fisetin on experimentally induced airway hyperreactivity. Pharm Jr. 2017.
- Kamei R. et al. A flavanone derivative from the Asian medicinal herb (Perilla frutescens) potently suppresses IgE-mediated immediate hypersensitivity reactions. Biochem Biophys Res Commun. 2017 Jan 29;483(1):674-679.
- Chen ML et al. Ethanol extract of Perilla frustescens suppresses allergen-specific Th2 responses and alleviates airway inflammation and hyperactivity in ovalbumin sensitive murine model of asthma. Evidence based Comp. and Alt. Med. 2015.
- Roschek B. et al. Nettle extract (Urtica dioica) affects key receptors and enzymes associated with allergic rhinitis. Phytother Res. 2009 Jul;23(7):920-6.
- Shakeri F, Gholamnezhad Z, Mégarbane B, Rezaee R, Boskabady MH. Gastrointestinal effects of Nigella sativa and its main constituent, thymoquinone: a review. Avicenna J Phytomed. 2016;6(1):9-20.
- Ikhsan M, Hiedayati N, Maeyama K, Nurwidya F. Nigella sativa as an anti-inflammatory agent in asthma. BMC Res Notes. 2018;11(1):744. Published 2018 Oct 19. doi:10.1186/s13104-018-3858-
